AcryMed is touting their latest innovation in wound healing: Dissolved oxygen delivery, via their Oxygenesys system:
Our research shows that these new devices deliver significant amounts of dissolved oxygen, which is the biologically relevant form” said Dr. Bruce Gibbins, Founder and Chief Technical Officer at AcryMed. “We conducted studies on human donor skin to show for the first time that through Oxygenesys TDO, sufficient oxygen penetrates deep into tissues to make up for the oxygen deficiency … read more
Keywords:
Oxygen therapy,
OxyGenesys,
AcryMed,
SilvaSorb,
Chronic wounds
AcryMed’s OxyGenesys for Wound O2 Delivery: Where It Stands in 2025
Original Post Date: August 2, 2018
Updated: June 4, 2025
Update Note: This post has been updated in June 2025 to provide the latest insights on OxyGenesys and to introduce NATROX O₂, a modern alternative for topical oxygen therapy in wound care. We’ve added new details to help you stay informed about the best options for managing chronic wounds.
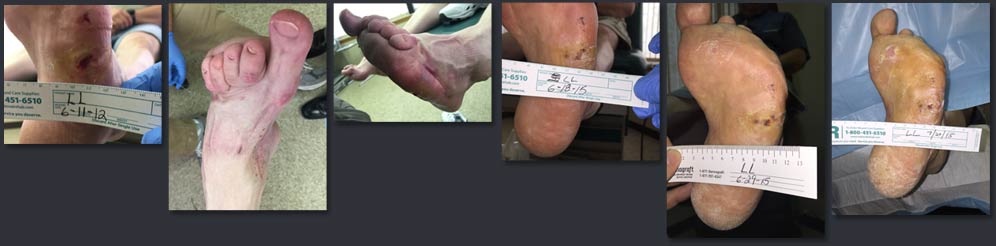
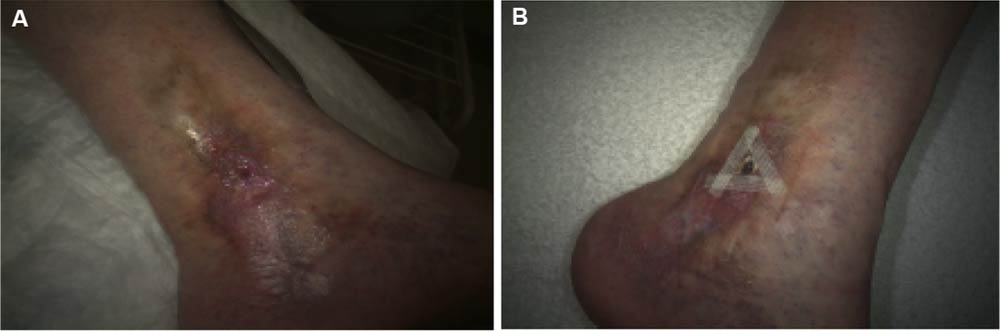
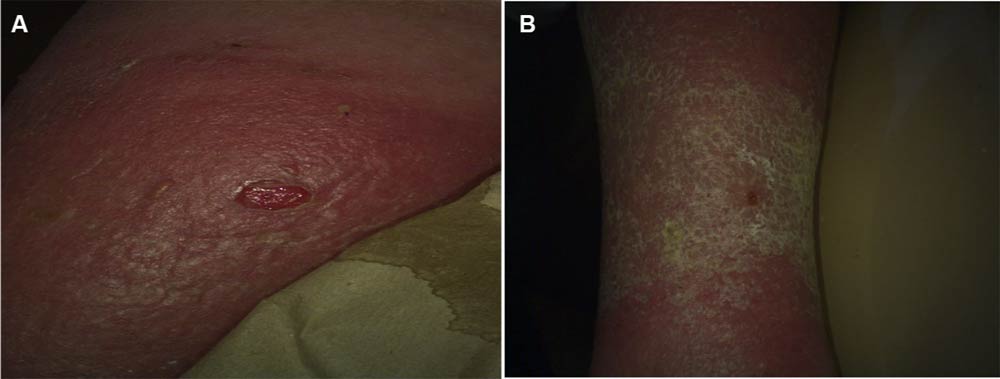
Oxygen is critical for wound healing, playing a key role in cell growth, infection prevention, and reducing inflammation. However, chronic wounds like diabetic foot ulcers or venous leg ulcers often suffer from hypoxia—low oxygen levels due to poor blood flow. This is where topical oxygen therapies (TOT) come in, delivering oxygen directly to the wound to support healing.
Back in 2018, we covered AcryMed’s OxyGenesys, a promising system for wound oxygen delivery. Let’s revisit OxyGenesys, explore its current status, and compare it to a leading alternative, NATROX O₂, which is making waves in 2025.
OxyGenesys: What We Knew in 2018
OxyGenesys was developed by AcryMed, a Beaverton, Oregon-based company focused on wound care innovations. Dr. Bruce Gibbins, AcryMed’s Founder and Chief Technical Officer, shared that OxyGenesys was designed to deliver “significant amounts of dissolved oxygen, which is the biologically relevant form” for wound healing.
AcryMed’s studies on human donor skin showed that OxyGenesys could penetrate deep into tissues, addressing oxygen deficiencies in chronic wounds. This was a big deal because deeper oxygen delivery could potentially accelerate healing, reduce infection risks, and improve outcomes for patients with hard-to-heal wounds.
At the time, OxyGenesys seemed like a game-changer, especially since topical oxygen therapy was gaining traction as a non-invasive way to treat chronic wounds. But what’s happened since then?
OxyGenesys in 2025: Is It Still Available?
Unfortunately, the trail for OxyGenesys goes cold after 2018. AcryMed was acquired by I-Flow Corporation in 2008 for $25 million, with the goal of expanding I-Flow’s wound care offerings. I-Flow was then bought by Kimberly-Clark Healthcare in 2009, which later became part of Owens & Minor.
Employee reviews on Glassdoor suggest AcryMed was shut down after these acquisitions, with the last update from 2015 mentioning its closure. There’s no recent public data on OxyGenesys—no new studies, product listings, or mentions in Owens & Minor’s current portfolio, which now focuses on brands like HALYARD and MediChoice.
A 2025 post on our site referenced an abdominoplasty trial involving OxyGenesys, but the results were inconclusive, showing no significant healing benefits. However, this trial focused on cosmetic surgery wounds, not chronic wounds, which may not align with OxyGenesys’ intended use.
Without updates from Owens & Minor or AcryMed, it’s likely that OxyGenesys is no longer available, possibly discontinued after AcryMed’s closure. If you have information on its current status, we’d love to hear from you in the comments!
A Modern Alternative: NATROX O₂
While OxyGenesys may no longer be an option, topical oxygen therapy remains a vital tool for wound care, and newer technologies have stepped up. One standout is NATROX O₂, developed by Inotec AMD Ltd., which shares OxyGenesys’ goal of delivering oxygen to wounds but with modern advancements and robust clinical evidence as of 2024.
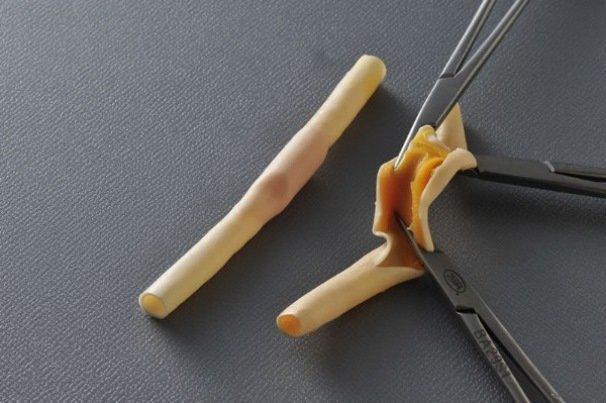
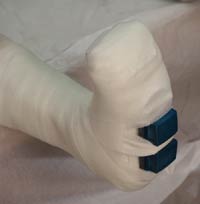
NATROX O₂ is a portable, battery-powered device that provides continuous topical oxygen therapy (cTOT) at a low flow rate of 11ml/hour. It includes an Oxygen Generator that produces pure, humidified oxygen from atmospheric air, and a sterile Oxygen Delivery System with a wheel-shaped design that conforms to the wound, allowing exudate to pass while optimizing oxygen diffusion.
Unlike older systems, NATROX O₂ is silent, lightweight, and designed for 24/7 use, making it practical for both home and clinical settings. It works with most secondary dressings, adding to its versatility.
The evidence for NATROX O₂ is compelling. A 2021 study showed a 71% greater healing rate for chronic wounds like diabetic foot ulcers compared to standard care alone. Patients also reported a 76% reduction in pain, and wounds saw a 73% greater size reduction.
In 2023, the Wound Healing Society gave cTOT a Level 1 evidence rating, and the American Diabetes Association included it in their guidelines for hard-to-heal wounds. NATROX O₂ has been successfully used in over 30 countries, with case studies showing faster healing, lower infection rates, and even limb salvage in severe cases.
Compared to OxyGenesys, NATROX O₂ likely offers a similar focus on sustained oxygen delivery to combat hypoxia, but with the advantage of being actively available and backed by recent data. While OxyGenesys emphasized deep tissue penetration, NATROX O₂’s continuous flow ensures a steady oxygen gradient, which may achieve similar benefits for chronic wound healing.
Why This Matters for Wound Care
Topical oxygen therapies like OxyGenesys and NATROX O₂ address a critical need in wound care: providing oxygen to wounds that traditional treatments can’t heal. If OxyGenesys is no longer available, NATROX O₂ offers a modern, evidence-based alternative that’s accessible today.
For patients, caregivers, and professionals visiting woundcareweekly.com, exploring options like NATROX O₂ can lead to better outcomes for chronic wounds. Interested in learning more about NATROX O₂? Visit their official site for details on how it works and how to access it for your wound care needs [Note: You can insert an affiliate link here if you join a program with NATROX O₂ or a distributor].
Stay tuned to woundcareweekly.com for more updates on wound care innovations.