A research team led by Professor Lim Chwee Teck from the National University of Singapore’s (NUS) Department of Biomedical Engineering and Institute for Health Innovation & Technology (iHealthtech), in collaboration with clinical partners from Singapore General Hospital, has developed a smart wearable sensor that can conduct real-time, point-of-care assessment of chronic wounds wirelessly via an app. A world’s first, the novel sensor technology can detect temperature, pH, bacteria type and inflammatory factors specific to chronic wounds within 15 minutes, hence enabling fast and accurate wound assessment … read more
Tag: diabetic foot ulcer
Probiotics accelerate wound healing in patients with diabetic foot ulcer
Patients with diabetic foot ulcer (DFU) who were given probiotic supplements for 12 weeks had faster wound healing and improved glycemic control compared with similar patients on placebo, according to researchers who recently published their results in Diabetes/Metabolism Research and Reviews.

Diabetic foot ulcers healed faster in patients given probiotics.
“Due to the increasing global antimicrobial drug resistance issues, the idea of probiotic consumption is interesting and pertinent because probiotics have the ability to strengthen the immune system, have anti-inflammatory effects, and therefore, could increase the wound healing process,” wrote lead co-author Zatollah Asemi, PhD … read more
Incidence, hospitalization and mortality and their changes over time in people with a first ever diabetic foot ulcer
Diabetic foot ulcers (DFUs) are a severe complication associated with diabetes, a precursor for amputation, and a major cause of patient suffering and high health-care costs.1,2 While the continuous efforts of multidisci-plinary foot clinics and preventive activities in primary care have reduced the incidence of major lower limb amputations in most countries, the prevention of DFUs remains a major challenge.3- 5 Over the years several risk factors associated with the development of a DFU have been discovered, but despite this, little is known about the factors leading directly to the first ever ulceration.6 Therefore, the predictive power of even seasoned cli-nicians in our experience remains low, and combined with the poorly reported, but relatively low, incidence of first ever DFUs, the possibilities for primary prevention is extremely limited.7 These challenges have led to re-current DFUs being studied far more than the first ever DFUs, but despite continuous improvements in healing … read more
Malta’s first space research touches back down on earth
Project seeking to innovate diabetic ulcer treatment
Led by associate professor of biomedical science at the University of Malta Joseph Borg, the Project Maleth team sent samples of micro-organisms that cause diabetic ulcers to the International Space Station (ISS), in a bid to analyse how the tissue will react under extreme conditions.
They hope that the information they glean from the results will be able to help patients by developing new ways to treat diabetes and its symptoms … Launched from Cape Canaveral in Florida on August 28, Project Maleth spent just over a month aboard the International Space Station … read more
Foot Revascularization Avoids Major Amputation in Persons with Diabetes and Ischaemic Foot Ulcers
The study aims to evaluate the effectiveness of foot revascularization in persons with diabetic foot ulcers (DFUs) and below-the-ankle (BTA) arterial disease. Consecutive patients referred for a new active ischaemic DFU requiring lower limb revascularization were considered. Among those, only patients with a BTA arterial disease were included. Revascularization procedures were retrospectively analysed: in the case of successful foot revascularization (recanalization of pedal artery, or plantar arteries or both) or not, patients were respectively divided in two groups, successful foot perfusion (SFP) and failed foot perfusion (FFP). Healing, minor and major amputation at 12 months of follow-up were evaluated and compared. Eighty patients (80) were included. The mean age was 70.5 ± 10.9 years, 55 (68.7%) were male, 72 (90%) were affected by type 2 diabetes with a mean duration of 22.7 ± 11.3 years. Overall 45 (56.2%) patients healed, 47 (58.7%) had minor amputation and 13 (16.2%) major amputation. Outcomes for SFP and FFP were respectively: healing … read more
Diabetic Foot Ulcer Prevention Strategies
Diabetic foot ulcers (DFUs) may affect up to 25% of people with diabetes at some point in their lifetime. Once a person has developed a DFU, there is a 50% chance the ulcer will become infected.1 DFUs are also among the leading causes of amputation.2
Wound care specialists encounter DFUs regularly in the clinic, and these wounds can be very difficult to treat because of the underlying metabolic insufficiency. This blog provides a guide to current best practices with regard to DFUs and prevention … read more
Combined Regenerative Approach for a Complex Lower Extremity Wound
More than 400 million patients worldwide are affected by diabetes; over their lifetime, at least 25% will develop foot ulcers that often result in high rates of nonhealing wounds and amputation. The authors present the case of a 43-year-old female patient with multiple comorbidities who presented with a large (8 cm x 4 cm), noninfected, hindfoot plantar ulcer that extended down to the bone and calcaneus. Over 2 weeks, the patient was successfully treated using a combination of an acellular dermal matrix, nanofat grafting, and negative pressure wound therapy, lessening the effects of the ulcer on the patient’s quality of life and achieving limb salvage. Utilizing the regenerative procedures described herein may improve patient care and decrease costs … read more
The Biomechanics of Diabetic Foot Amputation
According to the International Diabetes Federation, approximately 463 million adults live with diabetes mellitus (DM), a number projected to increase to 700 million by 2045; a diabetic foot ulcer (DFU) will occur in about 15% of that population. Multiple factors contribute to the development of those wounds including diabetic peripheral neuropathy, biomechanical imbalances, trauma, and peripheral vascular disease. In addition, 85% of all lower limb amputations in patients with diabetes are preceded by a DFU resulting in significant biomechanical challenges for these patients, many of who never become ambulatory again. Prior to surgical intervention, patients come with inherited and acquired biomechanical imbalances or weaknesses such as equinus, severe pronation/supination, mid and forefoot deformities, and muscle weakness unrelated to their other diseases. Surgeons may not take these into consideration when making decisions about amputation level … read more
Take A Load Off: Offloading Tips And Pearls In Wound Care
Diabetic foot ulcerations (DFUs) affect approximately 26 million people worldwide, with a staggering 2.5 times increased risk of death at five years.1-3 While many etiologies and conditions contribute to a wound, offloading is crucial to solving the wound healing puzzle.
In some literature, offloading is the most important aspect of DFU treatment in patients with neuropathy.4-6 The thought behind offloading is relief of mechanical and abnormal stresses that the foot experiences from a loss of protective sensation. This combination results in tissue damage, thought to lead to many DFUs.1,4,7 Specifically, mechanical stress is due to increased plantar pressure and shearing forces during the gait cycle, causing repetitive microtrauma … read more
Oxygen-delivering hydrogel accelerates diabetic wound healing
About one-fourth of people with diabetes develop painful foot ulcers, which are slow to heal due to low oxygen in the wound from impaired blood vessels and increased inflammation. These wounds can become chronic, leading to poor quality of life and potential amputation … ianjun Guan, professor of mechanical engineering and materials science at the McKelvey School of Engineering at Washington University in St. Louis, has developed a hydrogel that delivers oxygen to a wound, which decreases inflammation, helps remodel tissue and accelerates healing. Results of the work, which were in a mouse model, are published Aug. 28 in Science Advances. Ya Guan, a doctoral student, and Hong Niu, a postdoctoral research associate, both in Guan’s lab, are co-first authors … read more
A report of 12 months’ of data collected from a diabetic foot clinic at a public hospital in Phnom Penh, Cambodia
This report interprets data gathered from a diabetic foot ulcer clinic in an outpatient department of a public hospital in Phnom Penh, Cambodia. The data were gathered between September 2019 and August 2020 and were entered into a Microsoft Excel™ spreadsheet. It gives basic demographic information of Cambodian patients with diabetic foot ulceration and provides data that can be used to measure any future research or audit. The data collection timeframe … read more
Significant Reductions in Amputations, Emergency Visits, and Hospital Readmissions Associated with Advanced Treatment Using Skin Substitute Products …
MiMedx Group, Inc. (Nasdaq: MDXG) (“MIMEDX” or the “Company”), an industry leader in utilizing amniotic tissue as a platform for regenerative medicine, today announced publication of its peer-reviewed study in the Journal of Wound Care (JWC), addressing the observed impact of Advanced Treatment (AT) using all high-cost skin substitute products in lower extremity diabetic ulcers (LEDUs) based on data from the Medicare Limited Dataset (October 1, 2015 through October 2, 2018). The study assessed outcome in patients receiving AT with all high-cost skin substitute products, as designated by the Centers for Medicare and Medicaid Services (CMS), for LEDUs versus No Advanced Treatment (NAT), and found that AT use could lead to a 42% reduction in major and minor amputations and all related costs, compared to NAT. Further, the study highlights preferable outcomes when AT follows parameters for use (FPFU), underscoring the importance of early treatment with regular intervals and well-defined treatment guidelines … read more
Medicinal Plants as Efficacious Agents for Diabetic Foot Ulcers: A Systematic Review of Clinical Studies
A diabetic foot ulcer (DFU) is a chronic, nonhealing wound that occurs in approximately 15% to 25% of patients with diabetes, and amputation is necessary in approximately 5% to 24% of these patients. Medicinal plants have demonstrated promising wound healing activities in animal models of DFUs as well as in clinical studies. These plants, which are described as medicinal in different regions of the world, are not considered to be standard medicinal treatments in Western medicine at this time. Some medicinal products, such as bromelain—an herbal protease currently used for enzymatic debridement of wounds—have been obtained from plants, showing the important role of these natural products as sources of wound healing agents. This paper aims to review clinical studies on the effects of medicinal plants in patients with DFUs based on the improvement of local and systemic parameters related to wound healing. Electronic databases including PubMed, Scopus, and Cochrane Library were searched for studies from inception through May 2019 using the keywords “diabetic foot ulcer” … read more
SkinTE® Met Primary and Secondary Endpoints in Final Analysis from Diabetic Foot Ulcer Trial
SALT LAKE CITY–(BUSINESS WIRE)–PolarityTE, Inc. (Nasdaq: PTE) today announced final data from a multi-center randomized controlled trial evaluating treatment of Diabetic Foot Ulcers (DFU) with its investigational product SkinTE® plus standard of care (SOC) vs SOC alone (NCT03881254). The trial met the primary endpoint of wound closure at 12 weeks and secondary endpoint of Percent Area Reduction (PAR) assessed at 4, 6, 8, 10, and 12 weeks. 100 participants were evaluated across 13 sites with 50 participants receiving SkinTE plus SOC and 50 receiving SOC alone. PolarityTE is pleased to announce today the final analysis of the full data set, which includes:
- Primary Endpoint: 70% (35/50) of participants receiving SkinTE plus SOC had wound closure at 12 weeks versus 34% (17/50) of participants receiving SOC alone (p=0.00032)
- Secondary Endpoint: Percent Area Reduction (PAR) assessed at 4, 6, 8, 10, and 12 weeks was significantly greater for the SkinTE plus SOC treatment group vs SOC alone (p=0.009)
- 90% (45/50) of SkinTE plus SOC treated participants received a single application of SkinTE
- Treatment with SkinTE plus SOC increased the odds of wound closure by 5.37 times versus SOC (p=0.001)
Mean (SD) values for PAR at weeks 4, 6, 8, 10, and 12 by treatment group
|
Week |
SkinTE |
SOC |
|
4 |
74.0 (27.63) |
22.0 (149.92) |
|
6 |
82.9 (26.35) |
21.2 (160.60) |
|
8 |
80.7 (35.16) |
26.8 (147.42) |
|
10 |
79.7 (54.07) |
45.6 (114.18) |
|
12 |
84.3 (39.46) |
50.5 (92.24) |
Negative Pressure Wound Therapy Reduced Amputation Risk for Patient With Diabetic Wound
A patient with a diabetic foot wound who underwent negative pressure wound therapy experienced good healing, reduced amputation risk, and no wound infection, suggesting the treatment method could be effective in other patients with similar wounds.
A patient who received negative pressure wound therapy (NPWT) after undergoing surgical debridement for a diabetic wound saw improvements in healing capabilities and reduced risks of limb amputation, according to a recent case report published in SAGE Open Medical Case Reports.
The report lends further support to previously published research that has shown NPWT to be effective at decreasing healing time, reducing ulcer area, and increasing healing rates of ulcers. NPWT has also been shown to aid patients with foot ulcers in achieving complete ulcer closure better than advanced moist wound therapy … –
Multiple Interventions for Diabetic Foot Ulcer Treatment (MIDFUT) trial: benefits of involvement for patients and clinicians
Pragmatic diabetic foot ulcer research is key to enhancing clinical expertise and efficiency, patient experience and improved wound healing. Delivery of novel adjuvant therapies in a clinic setting can be challenging, both at clinical and organisational levels. There are many benefits to patients and clinicians from being involved in research. The aim of this article is to present the Multiple Interventions for Diabetic Foot Ulcer Treatment (MIDFUT) trial, describe its purpose, the project implementation and how it is overcoming the challenges of delivering novel therapies in a clinic setting, and the potential benefits to patients and staff … read more
Diabetic foot ulcer, the effect of resource-poor environments on healing time and direct cost: A cohort study during Syrian crisis
This study was intended to assess the healing time of diabetic foot ulcer (DFU) during what is considered one of the worst humanitarian crises of the 21st century. Researchers examined 1,747 DFUs from the main diabetic foot clinic in Damascus (2014-2019). They conducted SINBAD Classification to grade the severity of ulcers. This study’s findings demonstrate that the environment with resource-poor settings should be added to the traditional risk factors that delay the healing of DFUs for months or even years. There is a need for more studies to analyze low-cost materials that could be cost-effective in applying standard care to the diabetic foot … read more
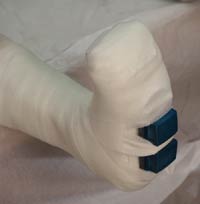
A Novel Method to Offload Neuropathic Ulcers of the Distal Phalanges in the Presence of First Ray Metatarsal Hypermobility
The standard practice to heal neuropathic ulcers on the toes is to offload the affected areas with special types of therapeutic footwear including shoes and boots to reduce the amount of pressure on the wound. Once healed, the individual wears custom insoles to prevent the development of new wounds. In our practice, we found that some newly healed wounds will reulcerate despite wearing therapeutic footwear. We devised a method to prevent and offload neuropathic foot ulcers on the distal phalanges in the presence of first ray metatarsal hypermobility, a common problem associated with the development of wounds … read more
DECREASING AMPUTATION, WORLDWIDE…BUT GREATER PREVALENCE AND MORTALITY FROM DIABETIC FOOT ULCERS (DFU)?
Here is a mashup of two manuscripts recently posted to the blog. While amputation appears to be reducing in OECD states, the risk for mortality secondary to DFU is high and may be getting higher … read more
Can Topical Oxygen Have An Impact On DFU Healing?
Data continue to accumulate for some role of topical oxygen (TOT) in tissue repair and wound healing. A study from Golledge and colleagues in Australia reveals some interesting developments.1 Their systematic review and meta-analysis examined evidence for the benefit of topical oxygen therapy in healing diabetic foot ulcers (DFUs) … read more
Keys To Addressing Forefoot Plantar Ulcerations
The Centers for Disease Control and Prevention (CDC) estimates one in ten Americans have diabetes and one in three have prediabetes … Diabetes is also increasing among younger populations and can lead to sleep apnea, cardiovascular disease, pulmonary disease and risk of cancer … One major complication of diabetes is diabetic peripheral neuropathy (DPN), seen in 50 percent of the geriatric population with diabetes … continue
T-Natural Killers and Interferon Gamma/Interleukin 4 in Augmentation of Infection in Foot Ulcer in Type 2 Diabetes
Epidemiology studies have shown that diabetes has the highest incidence of any chronic disease worldwide and is a huge threat to human health. Diabetes is clinically divided into types I and II.1 The prevalence of type II diabetes mellitus (T2DM) increases with age across all regions and income groups.2 Still, the prevalence is increasing in young age groups due to unhealthy life routines present since childhood … Insulin resistance (IR) associates with T2DM. Diabetes-related foot complications are important causes for disability worldwide. More than one-third of patients with diabetes worldwide will develop diabetic foot ulcer (DFU), which can progress to diabetic foot infection (DFI), and gangrene, consuming most of the healthcare costs dedicated for patients with diabetes. Around 17% of DFI will require amputation. Studies showed that patients with diabetes fear amputation more than death. The DFI patients will demand extensive debridement … continue
Expert Insight: Technology to Help Tackle Diabetic Foot Problems
As I’m sure you all know diabetic foot problems in this country and most western countries represent the commonest cause for patients with diabetes being admitted to hospital. And I think there is much we can do about this, and I really think that ulceration, as it’s so common and recurrence is so common, we should really redesign what we say when the patient is healed. Healing gives the impression that it’s gone away and will never come back. Thus in a recent review article[1] with my good friend David Armstrong, from the USA, and Sicco Bus from the Netherlands, we brought out the term remission rather than heal, because foot ulcers recur up to 40% in the first year and up to 60% after several more years. So we should be talking about the foot being in remission because it may recur.
Now what can we do about the foot in remission to prevent recurrence? And I think there’s a lot of exciting data coming through recently. First of all, not recently, it was Dr Paul Brand[2] who worked in leprosy, who observed that the insensitive foot in leprosy, and also in diabetes, tends to heat up before it breaks down. Therefore, the foot warms up because it becomes inflamed … read more
Corstrata Announces Availability of New Tech Empowered
Diabetic Foot Ulcer & Amputation Prevention Solution
SAVANNAH, GA. (PRWEB) JULY 10, 2018
CORSTRATA, a provider of digital healthcare IT solutions and services for wound management, announced today the availability of the company’s new Diabetic Foot Ulcer & Amputation Prevention Solution. The Solution is designed to prevent costly and complicated wounds from developing and is the first comprehensive program that leverages state-of-the-art technology and a team of top-tier Board Certified Wound Clinicians for the early detection of ulcers that often lead to hard-to-heal wounds and amputations among the growing U.S. diabetic population.
Diabetic foot ulcers (DFUs) are a common, limb-threatening and expensive complication of Type 1 and Type 2 diabetes. Today, more than 30M people in the U.S. have diabetes and more than 1.7M suffer from new DFUs per year with a 40% reulceration rate. 80K of these diabetics ultimately require an amputation and the risk of death at 5 years for DFU patients is 2.5 times as high as the risk for a patient with diabetes without a foot ulcer.
“The Corstrata Diabetic Foot Ulcer and Amputation Solution offers an important advancement in both the detection and prevention of one of the most costly and complex types of wounds to heal,” said Katherine Piette, Chief Executive Officer and Founder, Corstrata. “The mobile and remote monitoring technology combined with our deep clinical expertise in diabetic foot ulcer prevention and wound management, enable us to help payers and value-based care organizations significantly reduce their risk and costs associated with ulcerations in diabetic members.”
The Corstrata program is a comprehensive end-to-end technology-enabled solution that uses the HIPAA compliant, Corstrata Intervention & Engagement mobile app and the industry’s only FDA approved smart thermometric mat. The Solution is designed to help value-based care organizations and payers with the following:
- High-Risk Patient Identification
- Program Enrollment
- Daily Remote Patient Monitoring
- Member Engagement & Education
- Timely Evidenced-Based Intervention for Prevention of DFU
- Empowering Members for Self-Management
“Research indicates that the use of early detection technology, coupled with evidence-based interventions, can prevent 75% of foot ulcers in this high-risk population,” said Joseph Ebberwein, Chief Financial Officer and Founder, Corstrata. Lower extremity amputation studies and clinical trials have shown that Diabetic Foot Ulcer and Amputation prevention solutions can greatly reduce costly hospital visits and procedures associated with ulcerations and amputations, including:
- Reduction in Hospitalizations
- Decreased Hospital Days
- Reduction in Amputations
- Decreased Emergency Room Visits
- Decreased Foot Ulcer Recurrence
Corstrata was also recently named a semifinalist in the T1D Exchange 2018 Diabetes Innovation Challenge. A poster depicting the Corstrata DFU solution was showcased at the public event on May 21, 2018, at the Royal Sonesto Boston in Cambridge, MA.
Learn more about the Corstrata Diabetic Foot Ulcer and Amputation Prevention Solution at Corstrata.com/Diabetic-Foot-Ulcer-Prevention.
About Corstrata
Corstrata was founded in 2015 by two passionate healthcare experts with the goal of improving access to technology enabled, evidence-based care for patients with chronic wounds, which currently costs the U.S. $33B annually. Home health agencies, hospices, self-funded employers, clinically integrated networks of doctors and related practitioners (CINs), and third-party payers (Medicare Advantage, Medicaid MCOs) can benefit from Corstrata’s unique combination of professional expertise, digital technologies and telemedicine to treat wound patients and support practitioners anywhere, any time. The company delivers a Comprehensive Wound Care Management Program, Wound Patient Consultations, and specific services such as wound program assessment, formulary design, treatment guidelines assessment, wound documentation review, and practitioner education. Wound program development is available for Pressure Injury (Ulcer) Prevention and Management, Diabetic Foot Ulcer Prevention and Management, Ostomy Care and Management, and Palliative Wound Management. For more information about Corstrata, visit Corstrata.com.
Treatment of Diabetic Foot Ulcers
Diabetic wound is the most common cause of non-traumatic
lower extremity amputation, and response to traditional
interventions is poor in many patients. The lifetime risk of
developing an ulcer among diabetics is 25%, and recurrent
wounds are common after healing. Stigmatization, social
isolation, unemployment, and depression are some of the
negative consequence of Diabetic Foot Ulcer (DFU) on the
quality of life of diabetics. DFU adds a substantial economic
burden to afflicted patients and health systems, primarily
attributable to frequent hospitalization, medication, surgical
procedures, amputation, prosthesis, rehabilitation, and loss of
productivity … read more
Diabetic Foot Ulcer Prevention System (DFUPS)
The purpose of this study is to investigate whether regular measurement of skin foot temperature with a novel device (DFUPS) will prevent ulcer recurrence in diabetic patients at high risk of foot ulceration. It is planned to regularly measure the temperature of the feet of people with diabetes who have already had a foot ulcer which has subsequently healed. These measurements should allow the identification of hotspots on the foot and may be helpful when advising about ulcer risk and providing preventative treatment. It is hoped to find out whether the regular use of thermal images taken with the DFUPS device together with standard foot treatment may reduce the number of people with diabetes developing ulcers or even prevent foot ulcers … read more
Heberprot-P: a novel product for treating advanced diabetic foot ulcer
Diabetic foot ulcer is a principal diabetic complication. It has been shown that diabetic patients have decreased growth factor concentrations in their tissues, particularly epidermal growth factor. Growth factor shortage impairs wound healing, which leads to chronic nonhealing wounds and sometimes eventual amputation. Ischemic diabetic foot ulcer is the most difficult to treat and confers the highest amputation risk. Injecting epidermal growth factor deep into the wound bottom and contours encourages a more effective pharmacodynamic response in terms of granulation tissue growth and wound closure. Epidermal growth factor injected into the ulcer matrix may also result in association with extracellular matrix proteins, thus enhancing cell proliferation and migration. Heberprot-P is an innovative Cuban product containing recombinant human epidermal growth factor for peri- and intra-lesional infiltration; evidence reveals it accelerates healing of deep and complex ulcers, both ischemic and neuropathic, and reduces diabetes-related amputations. Clinical trials of Heberprot-P in patients with diabetic foot ulcers have shown that repeated local infiltration of this product can enhance healing of chronic wounds safely and efficaciously. As a result, Heberprot-P was registered in Cuba in 2006, and in 2007 was included in the National Basic Medications List and approved for marketing. It has been registered in 15 other countries, enabling treatment of more than 100,000 patients. Heberprot-P is a unique therapy for the most complicated and recalcitrant chronic wounds usually associated with high amputation risk. Local injection in complex diabetic wounds has demonstrated a favorable risk-benefit ratio by speeding healing, reducing recurrences and attenuating amputation risk. Further testing and deployment worldwide of Heberprot-P would provide an opportunity to assess the product’s potential to address an important unmet medical need.
Approval for commercialization of Heberprot-P® in Mexico
Havana, Cuba, May 4, 2018 – Heberprot-P® has been approved for commercialization in México. The Center for Genetic Engineering and Biotechnology (CIGB) is excited to announce regulatory approval of this innovative medicine indicated for advanced diabetic foot ulcer (DFU), which is expected to save thousands of people from lower limb amputation. The official approval date of Heberprot-P® was April 30th, 2018. Heberprot-P® stimulates granulation, accelerates DFU re-epithelization, and reduces healing time, surgical debridement, amputation risk, and recurrences. The intralesional infiltration of Heberprot-P® may be applied in combination with Good Wound Care (GWC), revascularization, and antibiotics. This medicine is an effective solution for an unmet medical need, a first in class product, unique worldwide, for DFU treatment. It is the only therapeutic choice available for advanced and complex DFU, reluctant to healing (grades 3, 4, and 5, according to Wagner’s classification).
Clinical experience derived from the intervention with Heberprot-P® in daily medical practice in Cuba was analyzed in 2013 in a study that reviewed the evolution of more than 2 000 patients as well as the pharmacovigilance of 1 788 patients, showing a 75% probability of granulation response, 61% healing rate, 71% amputation risk reduction, Bayes’ favorable factor (5.40), and complete granulation in 76% of ulcers in 5 weeks (Adv. Pharmacoepidem. 2013, 2 (2): 1000128; BMC Pharm. & Toxicol, 2013, 14: 44). The International Working Group of Diabetic Foot (IWGDF) evaluated results of the clinical trial performed with Heberprot-P® in Cuba and reported in 2009 as promising, highlighting the results obtained in only 2 weeks of treatment (Diabetes Metab Res Rev 2012; 28 (Suppl 1): 119-141).
In a later systematic review, clinical trials comparing the use of growth factors with GWC (Cochrane Database of Systematic Reviews 2015, Issue 10, Art. No. CD008548), the IWGDF’s evaluation was reported on all major issues and requirements of Heberprot-P® clinical trials in Cuba. Similar criteria were expressed by the IWGDF in the guidelines on DFU healing (IWGDF Guidance, 2015: 10). A fourth study reported similar observations on the intralesional EGF infiltration method: “… a highly significant difference between groups in the prevalence of granulation tissue after just 2 weeks” (Diabetes Metab Res Rev 2016; 32 (Suppl 1): 154- 168).
Results of clinical studies performed in Cuba, Russia, Turkey, Vietnam, Argentina, Mexico, and Ukraine were enough to demonstrate safety and efficacy profile of Heberprot-P®. This medicine has been used in more than 290 000 patients with diabetic foot ulcer (DFU) in Russia, Belarus, Georgia, Ukraine, Turkey, Algeria, China, Panama, Argentina, Cuba, Dominican Republic, Venezuela, Ecuador, Libya, Uruguay, Paraguay, Colombia, Guatemala, Philippines, Vietnam, Nicaragua, Saudi Arabia, Indonesia, Seychelles, Saint Lucia, Saint Vicente, Sri Lanka, Jordan, and Kuwait.
A national survey of health and nutrition in Mexico reported that prevalence of diabetes is 9.4% of total population, which sums up more than 11 million people, 9.1% of adult diabetic suffers DFU, and amputation is indicated to 5.5% of adult diabetics (National Survey of Health and Nutrition, INEGI 2016). According to recent reports, lower limb amputation is the unique alternative for 45% of diabetics with advanced DFU in Mexico (Diabet. Foot. Ankle. 2017 Sep 6, 8 (1): 1367210). In a previous study, similar results were reported: 42% patients with advanced DFU required major amputation (Wound Repair & Regen. 24 (5): 923-927).
Written by Jose A. Buxado, MSc., Assistant Researcher, CIGB.
The Center for Genetic Engineering and Biotechnology of Havana is an institution devoted to research, development, manufacturing, and commercialization of products and technology derived from life science.
Alyane Vazquez González, BA., Communication & Media, e-mail: alyane.vazquez@cigb.edu.cu
. Ave 31 e/ 158 y 190, Playa, P.O. Box 6162, Habana 10600, Cuba.
This release was published on openPR.
An evaluation of an ultrasonic debridement system
in patients with diabetic foot ulcers: a case series
Ferdinando CampitielloMD , Manfredi ManconeMD , Angela Della CorteMD , Raffaella GuernieroMD , Silvestro Canonico
Objective:
This study evaluated the use of ultrasonic debridement in patients with diabetic foot ulcers (DFU).
Method:
In this prospective, single-arm, open-label study, all patients with DFUs underwent wound debridement by ultrasonic debridement system (SonicOne OR Ultrasonic debridement system). Wherever possible, the edges were approximated by means of stitches. In other cases, the surgical breach healed by secondary intention, or a partial thickness skin graft (with or without Integra Dermal Regeneration Template or Integra Flowable Wound Matrix) was applied, and subsequently healed by primary intention … read more
Caring for the Diabetic Foot in Long-Term Care Facilities
By Susan M. Cleveland, BSN, RN, WCC, CDP, NADONA Board Secretary
As a Director of Nursing (DON) in a long-term care facility, do you know where the awareness level of diabetes and its complications is for your staff? Do they realize diabetes doesn’t stop? It is 24/7, 365 days a year. Knowing this reality of diabetes and understanding the disease process may assist with preventing serious health problems such as heart disease, stroke, blindness, kidney disease, and nerve damage that can lead to amputation.
Education is key. We cannot talk about this enough. Assuming someone knows or that common sense will tell people how to take care of these residents is a huge mistake. I don’t believe in common sense; I believe in common knowledge, but it is only common once it is taught. So, teach about diabetes and the care of residents with diabetes often.
Knowing the Risk of Diabetic Foot Ulcers and Diabetic Peripheral Neuropathy
In 2015, 30.3 million Americans, or 9.4% of the population, had diabetes. Approximately 1.25 million American children and adults have type 1 diabetes. The percentage of Americans age 65 and older remains high, at 25.2%, or 12.0 million seniors (diagnosed and undiagnosed).1Diabetic foot ulcer (DFU) is the number one risk factor contributing to non-traumatic foot amputations in persons with diabetes. Limb amputations are preceded by DFUs 58% of the time. The primary risk factor for the DFU is loss of protective sensations or diabetic peripheral neuropathy (DPN) … read more
Ultrasonic debridement system in patients with diabetic foot ulcers
A case series
Objective:
This study evaluated the use of ultrasonic debridement in patients with diabetic foot ulcers (DFU).
Method:
In this prospective, single-arm, open-label study, all patients with DFUs underwent wound debridement by ultrasonic debridement system (SonicOne OR Ultrasonic debridement system). Wherever possible, the edges were approximated by means of stitches. In other cases, the surgical breach healed by secondary intention, or a partial thickness skin graft (with or without Integra Dermal Regeneration Template or Integra Flowable Wound Matrix) was applied, and subsequently healed by primary intention … read more
The Neuropathic Diabetic Foot Ulcer Microbiome Is Associated With Clinical Factors
Nonhealing diabetic foot ulcers (DFUs) are a common and costly complication of diabetes. Microbial burden, or “bioburden,” is believed to underlie delayed healing, although little is known of those clinical factors that may influence microbial load, diversity, and/or pathogenicity. We profiled the microbiomes of neuropathic nonischemic DFUs without clinical evidence of infection in 52 individuals using high-throughput sequencing of the bacterial 16S ribosomal RNA gene. Comparatively, wound cultures, the standard diagnostic in the clinic, vastly underrepresent microbial load, microbial diversity, and the presence of potential pathogens. DFU microbiomes were heterogeneous, even in our tightly restricted study population, but partitioned into three clusters distinguished primarily by dominant bacteria and diversity. Ulcer depth was associated with ulcer cluster, positively correlated with abundance of anaerobic bacteria, and negatively correlated with abundance of Staphylococcus. Ulcer duration was positively correlated with bacterial diversity, species richness, and relative abundance of Proteobacteria, but was negatively correlated with relative abundance of Staphylococcus. Finally, poor glycemic control was associated with ulcer cluster, with poorest median glycemic control concentrating to Staphylococcus-rich and Streptococcus-rich ulcer clusters. Analyses of microbial community membership and structure may provide the most useful metrics in prospective studies to delineate problematic bioburden from benign colonization that can then be used to drive clinical treatment … read more
Evaluation of the WIfI classification system in older patients with diabetes
There are numerous factors that have an impact on diabetic foot ulcer (DFU) healing, among them critical limb ischaemia (CLI) — a term that was not intended to include patients with diabetic foot wounds and neuropathy. The Society for Vascular Surgery, therefore, created a new classification system for threatened lower extremities in which the severity of ulceration and severity of limb ischaemia are both graded. They also added a grade or classification scheme for infection.
The need to reconsider how the threatened limb is classified is clear. Ischaemia, while of fundamental importance, is but one component among a triad of major factors that place a limb at risk for amputation. The proposed Society for Vascular Surgery Lower Extremity Threatened Limb Classification System is based on grading each of the three major factors: Wound extent, degree of Ischaemia, and foot Infection, or WIfI (Mills et al, 2014). The implementation of this classification system is intended to permit more meaningful analysis of outcomes for various forms of therapy in this challenging and complex heterogeneous population. During the 1990s, most DFUs were considered neuropathic (Armstrong et al, 2011). The Eurodiale Study, which included 1,229 patients presenting with a new DFU between September 2003 and October 2004, found non-plantar ulcers to be most frequent type of ulcers in this group … read more
Caring for the Diabetic Foot in Long-Term Care Facilities
by Susan M. Cleveland, BSN, RN, WCC, CDP, NADONA Board Secretary
As a Director of Nursing (DON) in a long-term care facility, do you know where the awareness level of diabetes and its complications is for your staff? Do they realize diabetes doesn’t stop? It is 24/7, 365 days a year. Knowing this reality of diabetes and understanding the disease process may assist with preventing serious health problems such as heart disease, stroke, blindness, kidney disease, and nerve damage that can lead to amputation.
Education is key. We cannot talk about this enough. Assuming someone knows or that common sense will tell people how to take care of these residents is a huge mistake. I don’t believe in common sense; I believe in common knowledge, but it is only common once it is taught. So, teach about diabetes and the care of residents with diabetes often.
Knowing the Risk of Diabetic Foot Ulcers and Diabetic Peripheral Neuropathy
In 2015, 30.3 million Americans, or 9.4% of the population, had diabetes. Approximately 1.25 million American children and adults have type 1 diabetes … read more
Diabetic Wound Healing and LED Irradiation
Introduction: Light-Emitting Diode Therapy for Chronic Non-Healing Diabetic Wounds
Diabetes mellitus is frequently associated with chronic non-healing wounds, many of which result in amputation. The combination of peripheral vascular disease, neuropathy, and impaired immune function contributes to a higher risk of injury and deficiency in healing. Wound healing is a complex process comprising eight important factors: (1) collagen synthesis, (2) cell migration, (3) cell cycle and differentiation, (4) angiogenesis and growth hormone, (5) blood clotting, (6) extracellular matrix and focal adhesion, (7) calcium ion signaling, and (8) immune and inflammatory response. In the diabetic cell, all these processes malfunction, with the exception of collagen synthesis, cell migration, and cell cycle or differentiation.
Previous studies found an association between diabetes and the precursor protein pro-opiomelanocortin (POMC) gene. POMC is normally expressed in pituitary melanotroph and corticotroph cells and functions to control body weight. Studies have suggested that a mutation in the POMC gene leads to early-onset type 2 diabetes and obesity. This correlation is under investigation for its potential use in diabetic therapy.
Light-emitting diode (LED) phototherapy at 660 and 890nm has been shown to significantly accelerate wound healing in normal, healthy patients. This therapy works through molecules with porphyrin structures that are able to trap photon energy and subsequently activate downstream processes. The current study investigated the results of a range of different LED phototherapies on gene expression and cellular function of diabetic cells compared with normal, healthy cells … read more
Foot Sensation Testing in the Patient With Diabetes
Abstract: Introduction. Sensory testing of patients with diabetes is an integral part of preventing new and recurrent wounds. The Semmes-Weinstein monofilament (SWM) test is considered the gold standard to screen for loss of protective sensation; however, the authors’ experience has shown that it is not only time consuming, but is of negligible value for a patient with a diabetic foot ulcer (DFU).
Methods. This article discusses the shortfalls with regard to the SWM test and reviews other techniques for sensory evaluation. In addition, the Quick & Easy system is introduced, which combines sensory assessment with guidance for anesthesia requirements during wound debridements or other surgical interventions. Results. A scale ranging from grade 2 (normal sensation) to grade 0 (absent sensation) reflects the patient’s responses to wound manipulation, palpation of an underlying deformity, and/or evaluation of the difference between light touch sensation with the patient’s hands compared to the feet. For patients with total loss of sensation (grade 0), no anesthesia is needed for surgical procedures. If there is diminished sensation (grade 1), surgical intervention can be performed following administration of either topical or local anesthesia. For patients with normal sensation (grade 2), complete anesthesia of the surgical site will be required. A preliminary observation was conducted on 50 patients with DFUs using the Quick & Easy system. Anesthetic requirements were accurately predicted in all cases without the need to modify the type of anesthesia during the procedure. Conclusion. The Quick & Easy system serves as a simple sensory evaluation for a patient with a DFU and provides valuable anesthesia guidance for wound care procedures … read more
The Heels Trial – heel costs for ulcers of the heel in diabetes
Professor Fran Game – The Heels Trial – heel costs for ulcers of the heel in diabetes (TVS 2017 – Edgbaston Stadium)
Living with a Diabetic Foot Ulcer
Patient Perspective:
An Interview with Robert S. Meyer by Janet L. Kuhnke Robert Meyer lives with diabetes and a foot ulcer. He has attended multiple Wounds Canada events as both a speaker and to learn more about how he can manage his condition, heal his wound and prevent further foot complications. He is interviewed here by wound care clinician and educator Janet Kuhnke.
Janet L. Kuhnke: Robert, you attended the fall 2017 Wounds Canada conference in Mississauga, Ontario. Can you tell me what this was like for you as a patient?
Robert S. Meyer: I was there as a patient and a speaker, but it was not until I got back home that the depth of my message sank in. First, I wanted to do my talk as a tribute to my mother, who had a nasty death due to the complications of diabetes. Second, if my message could help someone, it would be worth it all. Not just for other patients but for other service providers who need to find their own inner voice and become advocates for themselves or others, no matter the issue. Third, telling my story has a profound impact on my own healing journey. Now I know why victims of trauma need to tell their story as part of their healing. The important part is knowing that someone has listened and heard … read more
Stratatech Begins Test of Engineered Skin for Diabetic Foot Ulcers
Stratatech is moving forward with tests of a genetically engineered human skin that could heal the sores and wounds many diabetic patients get on their feet.
Madison, WI-based Stratatech, a subsidiary of U.K.-based Mallinckrodt (NYSE: MNK), said Wednesday that it had enrolled the first patient in a study of the skin tissue, called ExpressGraft-C9T1.
Stratatech said the ExpressGraft skin tissue builds on some of the same technologies the company pioneered in developing StrataGraft, its flagship skin replacement product. StrataGraft is cell-based skin tissue designed to coax the bodies of burn patients into regenerating skin … read more
True impact of diabetic foot ulcers
The prognosis for people with an infected diabetic foot ulcer is worse than was previously thought, according to new research … More than half the patients in the research study did not see their ulcer heal over a year — and one in seven had to have part or all of their foot amputated … Foot ulcers are open wounds and they affect around a quarter of the 3.3 million people in the UK living with diabetes … The wounds develop because diabetes damages the nerves and blood vessels in the feet … These wounds are chronic, slow to heal and prone to infection, and it is infection that normally leads to some of the severe consequences such as losing a limb or multiple amputations … read more
Diabetic foot ulcers heal faster with probiotic supplementation
Findings from a randomized controlled trial revealed that patients with a diabetic foot ulcer, who received probiotic supplementation for 12 weeks, experienced faster wound healing coupled with an improved glycemic and lipid profile compared with patients assigned a placebo … read more.
New Study, Same Conclusion …
New Study, Same Conclusion. It is time to take another look at Total Contact Casting
Total Contact Cast
The most recent and perhaps the most conclusive study of for treatment of the diabetic foot is a collaboration of three prominent organizations, The Society for Vascular Surgery, the American Podiatric Medical Association and the Society for Vascular Medicine. The guidelines, “The Management of the Diabetic Foot,” were developed after three years of studies and are published online and in print in the Journal for Vascular Surgery. Dr. Anil P. Hingorani is the lead author that researched and wrote the guidelines. With diabetes a major worldwide problem and little data on treatments, the need for detailed, diabetic foot clinical guidelines from multiple disciplines was great, said Hingorani.
The committee synthesized the points of view of the three different medical professions by researching one another’s treatment protocols. Vascular surgeons and vascular medicine specialists read literature from podiatry and vice versa, for example, and all participants concentrated on infectious disease control and guidelines, a large component of the finished document. Collaboration was key, Hingorani said. “We had multiple disciplines looking at the problem to bring the best information from each field to develop the guidelines,” he said, though only limited “high-quality evidence” was available for many of the critical questions.
One of the findings that physicians may find surprising, it was the importance of the total contact cast in the treatment of plantar diabetic foot ulcers, which the committee found was is supported by robust data. Off-loading takes all direct pressure off the ulcer through use of a total contact cast. “total contact casting is so under-utilized,” Hingorani said. “I think some surgeons may find it surprising and it may raise a few eyebrows. Many surgeons are not aware of how strong the evidence is for total contact casting. It is not new but not widely understood or implemented.”
read more
Probiotic supplementation aids wound healing in diabetic foot ulcer
Patients with a diabetic foot ulcer who received probiotic supplementation for 12 weeks experienced faster wound healing coupled with an improved glycemic and lipid profile compared with patients assigned placebo, according to findings from a randomized controlled trial.
Sima Mohseni, of the infectious diseases and tropical medicine research center at Babol University of Medical Sciences in Iran, and colleagues analyzed data from 60 adults aged 40 years to 85 years with grade 3 diabetic foot ulcer, who randomly received either probiotic supplementation (n = 30) or placebo (n = 30) daily for 12 weeks between March and June 2016. Probiotic capsules contained lactobacillus acidophilus, lactobacillus casei, lactobacillus fermentum and Bifidobacterium bifidum. All participants also underwent standard treatment for wound care … read more
Lower Extremity Amputation and Reamputation Predictors ….
Review: Lower Extremity Amputation and Reamputation Predictors in Patients with Diabetic Foot Wounds
A major concern in managing patients with diabetes is their susceptibility to acquiring ulcers in their feet. If these patients are not careful, these ulcers may become infected and eventually lead to additional sequelae, ending in lower extremity amputation. The focus of this study was to determine the major factors of lower extremity amputation in the diabetic foot, in hopes that clinicians may be able to reduce the rate of amputations more effectively.
The authors performed a retrospective review of the records of 132 consecutive patients who had already received a lower extremity amputation or reamputation as a result of diabetic wounds. All patients had been diagnosed with diabetes mellitus type 2, and demographic and clinical data were collected on all of them. These data included age, sex, cigarette smoking history, duration of diabetes, diabetic comorbidities (nephropathy, neuropathy), general comorbidities (peripheral artery disease, hypertension, hyperlipidemia, malignancy), leukocytosis, wound infection status, and culture microorganism and antibiogram results. The side and level of amputation or reamputation were also recorded. Only those patients with wounds of a Wagner-Meggitt classification of 3 to 6 were included … read more
Reexamining The Gold Standard For Offloading Of DFUs
Although the total contact cast can be effective for offloading diabetic foot ulcers, it is not in wide usage. These authors assert the gold standard for offloading lies in the non-removability of the device and offer a closer look at the merits of transitional offloading.
According to the American Diabetes Association, there are approximately 29.1 million Americans, or 9.3 percent of the population, who suffer from diabetes.1 Twenty-one million of these people have already been diagnosed with the disease and 8.1 million remain undiagnosed.
This number, although large, pales in comparison with the 86 million Americans who have been classified as “pre-diabetic” and who are at risk of having diabetes in the near future.1 Each year, 1.7 million Americans 20 years of age or older add to this number. This amounts to 4,660 people per day or one new patient with diabetes every 19 seconds. A full 25.9 percent of Americans age 65 or older suffer from diabetes and its complications. Almost twice as many American Indians (15.9 percent) and African-Americans (13.2 percent) develop the disease as Caucasians (7.6 percent) with Hispanics close behind (12.8 percent). Asian-Americans are not spared as 9 percent of this population will develop the disease and its many complications.
Glycosylation affects all organ systems and leads to complications such as dyslipidemia with an increased incidence of hypertension, and systemic vascular disease. It also leads to the development of a progressive ascending peripheral neuropathy with a loss of sensation and sweat gland function. This in turn leads to ulceration and, in some cases, amputation when infection of the wounds goes unchecked by an immune system that is also compromised by the process …
read more
Research reveals the true impact of diabetic foot ulcers
The prognosis for people with an infected diabetic foot ulcer is worse than was previously thought, according to new research.
More than half the patients in the research study did not see their ulcer heal over a year – and one in seven had to have part or all of their foot amputated.
Foot ulcers are open wounds and they affect around a quarter of the 3.3 million people in the UK living with diabetes.
The wounds develop because diabetes damages the nerves and blood vessels in the feet.
These wounds are chronic, slow to heal and prone to infection, and it is infection that normally leads to some of the severe consequences such as losing a limb or multiple amputations.
The research, led by Professor Andrea Nelson at the University of Leeds, set out to examine the outcomes for people with infected diabetic foot ulcers and the results underline the need for people at risk of foot ulcers to be closely monitored.