the treatment of chronic nonhealing ulcers: a prospective case series
Introduction Millions suffer from diffcult to heal ulcers worldwide. The incidence of chronic ulcers is increasing rapidly, fueled by an aging population, rising incidence in obesity, diabetes, and venous insuffciency. Diabetic foot ulcers (DFUs), VLUs, and nonhealing postsurgical wounds are among the most frequently encountered ulcers in wound care practice. In the United States, over 4.3 million diabetic patients will develop a DFU in their lifetime, and ~2.5 million individuals suffer from VLUs. DFUs add 1–4 $9–$13 billion to the direct yearly cost associated with diabetes itself. The annual 5 cost of VLUs is $2.5–$3.5 billion. Nonhealing surgical wounds are also commonly 6 seen in wound care clinics. Surgical wounds pose an increased risk for infection and contribute to the growing economic burden of wound care management.
In recent years, several clinical trials have been conducted to investigate products derived from human amniotic membranes (HAMs) as adjunctive therapies to accelerate of different layers – the epithelium, basement membrane, and stroma – and these layers further consist of three contiguous but distinct layers – the inner compact layer, the middle fbroblast layer, and the outermost spongy layer. The HAM has been shown to have anti-infammatory, antifbrotic, antiangiogenic as well as antimicrobial properties. Research has confrmed that growth factors present in amniotic membranes can induce angiogenesis and human dermal fbroblast proliferation as well as recruit multiple stem cells relevant to wound repair and regeneration. 9,10
A fresh hypothermically stored amniotic allograft (HSAM) may improve healing rates by preserving growth factors and living cells, including stem cells, as well as retaining the membrane’s native structure. HSAM is aseptically processed and stored in a proprietary hypothermic storage solution using the Allofresh™ (Organogenesis, Canton, MA, sisting of topical antimicrobials. His comorbidities consisted USA) process. 13
Methods
A case study was conducted to evaluate an HSAM (Organogenesis) in the treatment of chronic wounds. Information was collected on patient demographics, wound type, wound location, age of wound, comorbidities, previous treatments, and current treatments. All patients were informed of study procedures and consented to have their case details and any accompanying photographs published. Digital planimetry (ARANZ Medical, Christchurch, New Zealand) was used ateach visit to record the wound surface area. Previous and current treatments were recorded. Two of the patients presented with VLU and one had a postsurgical wound.
The VLU patients had previously received compression, and one patient had also received negative pressure wound therapy. The one with a surgical wound had received a variety of previous therapies, including topical silver, Hydrofera Blue, and topical antibiotics. The age of the wounds for the VLUs were 2–3 weeks, while the surgical wound was 5 months. Comorbidities for the VLUs consisted of venous insuffciency, diabetes, arthritis, osteomyelitis to ulcer location, hypertension, and lymphedema. Comorbidities for the surgical wound patient consisted of arthritis and hypertension. The new treatment regimen consisted of HSAM covered with a knotted cellulose acetate fabric dressing (Adaptic ; Acelity, San Antonio, TX, USA) and appropriate standard of care, including offoading, multilayer compression, and of care, including offoading, multilayer compression, and surgical debridement.
Findings
Case 1
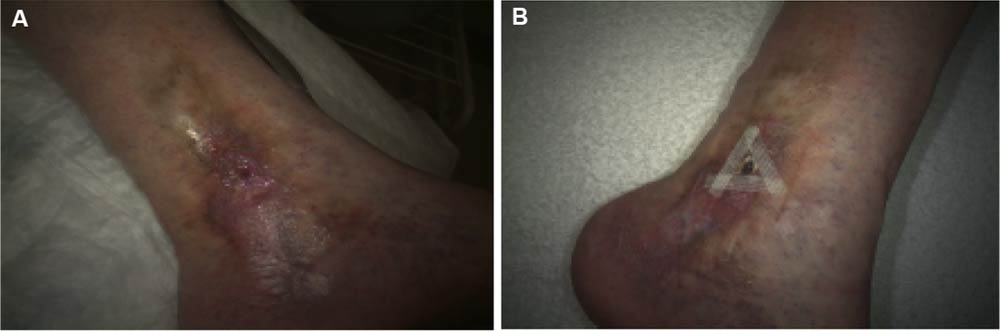
A 62-year-old patient presented to the wound clinic with a postop foot wound (nondiabetic), right foot dorsum. The duration of the wound was 5 months, with previous treatments consisting of topical antimicrobials. His comorbidities consisted of arthritis and hypertension. On day 0, the wound area size measured 3.3 cm , with 50% granulation, 10% fbrin, 40% slough, and a moderate amount of light red/pink serosanguineous drainage. Moderate edema was present. A 2.5 cm × 2.5 cm HSAM was applied and fxed in place using Steri-Strips™ (McKesson Medical-Surgical, Londonderry, NH, USA). On day 21, the wound area reduced to 2.9 cm2, a 12.12% reduction. There was an increase in the percentage of granulation tissue as well. By day 42, the wound area size had reduced by 81.82% with 100% granulation, and healed on day 71 (Figure 1).

Figure 1 Case 1 surgical wound.
Note: (A) Day 0, 3.3 cm2 ; (B) day 71, 0 cm2.
Case 2
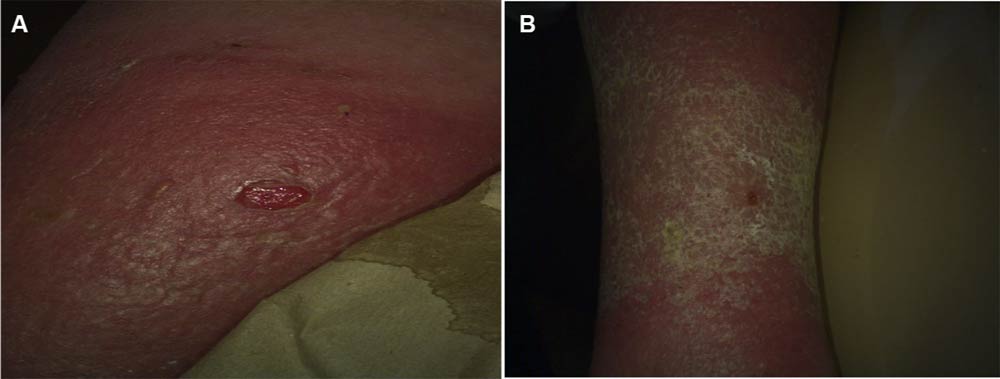
A 57-year-old patient presented with a left lower extremity VLU on the medial malleolus. The wound had been present for 8 weeks. The treatment thus far consisted of compression and topical antimicrobials. His past medical history included chronic venous insuffciency, peripheral vascular disease, deep vein thrombosis, and hyperlipidemia. On day 0, the wound area measured 0.3 cm . HSAM (2.5 cm x 2.5 cm) was applied and held in place with Steri-Strips™ ( McKesson Medical-Surgical) and compression wrap. On day 7, the wound was completed closed with no drainage (Figure 2).
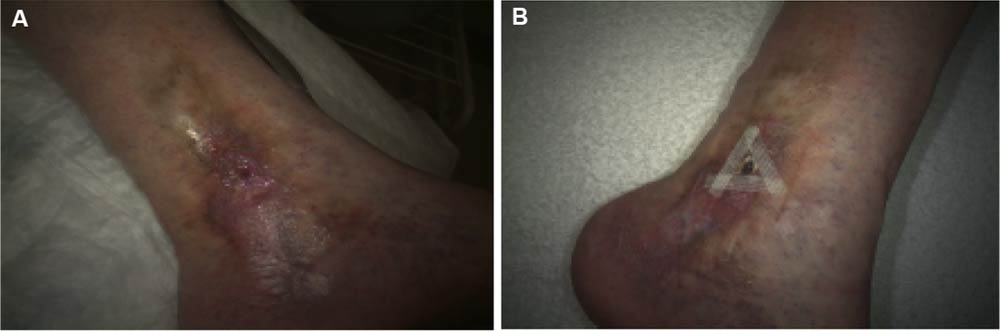
Figure 2 Case 2 venous leg ulcer.
Note: (A) Day 0, 0.3 cm2; (B) day 7, 0 cm2.
Case 3
A 70-year-old patient presented with a VLU on the medial right lower extremity. The wound had been present for 2 weeks. The medical history obtained from this patient revealed hypertension, lymphedema, type II diabetes, and chronic venous insuffciency. At the time of HSAM (2.5 cm × 2.5 cm) application, the wound area measured 1.0 cm . By day 7, the wound area was reduced to 0.4 cm , and by day 14, it achieved complete closure (Figure 3).
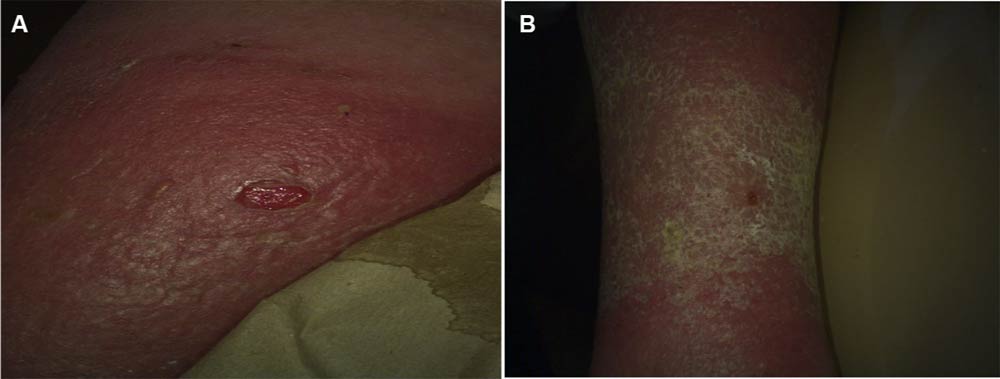
Figure 3 Case 3 venous leg ulcer.
Note: (A) Day 0, 1.0 cm2; (B) day 14, 0 cm2
Discussion
Prompt treatment of chronic ulcers is essential in preventing complications, reducing the cost of care, and lessening the economic burden on the health care system. In clinical studies, amniotic membranes have been shown to be effective in promoting healing in chronic wounds. Prior products consisted of dehydrated products. We postulated that fresh amniotic membrane would demonstrate even greater effect. Prior to embarking on large expensive clinical trials, we tried the fresh amniotic product on a few selected patients. Results from this study suggested that HSAM may be an effective treatment option for management of VLUs and other non-healing wounds. HSAM offers a new treatment alternative to promote healing in chronic wounds. This membrane contains numerous growth factors and cytokines. These growth factors are found to be released over an extended period and result in increased cellular migration, proliferation, and remodeling. Moreover, HSAM may reduce the long-term costs associated with the care of chronic ulcers by increasing the healing rate and lowering the risk of infection and complications This pilot case series was subsequently used to inform larger DFU and VLU trials that are ongoing at the time of this writing.
Original Article – Dovepress