Michael S. Miller DO, • Lindsey Markey RN, BSN • Regina Yoder RN • Kevin Powers DPM• TCC Kits provided by M-Med
Introduction:
It is well stated in the literature that Total Contact Casting (TCC) is a standard of care for off-loading of neuropathic ulcers of the plantar surface. Another standard of care is to provide a moist wound healing environment. Evidence to support appropriate wound dressings under TCC is currently unavailable despite recognition that the wound environment and thus the amount of drainage changes as the wound progresses towards healing. This pilot case series of three patients with plantar based diabetic neuropathic ulcers uses two dressings, a five layer silicone foam with absorbent polymer and moisture retentive backing dressing (SF)* for low to moderate drainage and a non-adherent super-absorbent (SAP)† polymer dressing for moderate to high exudate levels.
Clinical Problem:
Many TCC kits include a generic, open-cell, polyurethane foam dressing (OCF). These dressings do not absorb or retain fluid in a moderate to high exudate environment which can lead to maceration and non-healing. Furthermore, due to the high moisture vapor transmission rate of OCF, wounds with low exudate may experience desiccation and result in the development of slough and biofilm.1
Methods:
This pilot case series evaluates the performance of two dressings under a TCC‡. The 1st dressing is a five-layer silicone foam with super-absorbent polymer and moisture retentive backing for low to moderately exuding wounds (SF)*. The 2nd dressing is a non-adherent absorbent (SAP)† polymer dressing for moderate to high exudate levels. A total of 3 Wounds were assessed, cleansed, debrided if necessary, categorized by exudate level, and TCC was applied for 7 days. The expected outcomes were to avoid maceration, increase in healthy granulation/epithelial tissue, and achieve maximum wear time of TCC.
Results:
All three of the pilot cases healed completely in acceptable time with no untoward complications. The important feature was that the changes in the amounts of drainage which were identified as the healing progressed were compensated for by changing the dressings based on the amounts of exudate identified. This effectively minimized associated peri-wound maceration, damage to the increasing granulation tissue and improved tolerance of their feet to the total contact casting.
Conclusion:
TCC kits should consider including dressings for low-moderate and moderate-high exudate and cease adding the one-dressing-fits-all generic foam into the kit. Additionally, although foam dressings are lumped into single category, their individual traits such at total volume handling, exudate retention, and MVTR have erratic variation in function. The SF in this case series exceeded expectation and can be a standard of care unless exudate overwhelms the dressing in the 7 day expected wear. At that time, SAP should be used in place of SF to manage high exudate. Our experience is that this combination of dressings progresses wounds towards healing, enhances the clinical benefits and wear time of TCC, and decreases the potential for wound healing complications.
| Case History 1 45 year old Insulin-dependent diabetic male (IDDM) with a history of poor compliance presented with a plantar ulcer of 2 years duration. He had developed an acute Charcot’s Arthropathy, misdiagnosed as osteomyelitis and had surgery to remove “infected” bone. He had ongoing significant drainage with periwound skin maceration and no evidence of healing. |
Course of Treatment: Aggressive debridement of the ulcer was performed with identified bone at the base of the ulcer. However, further workup did not demonstrate osteomyelitis. He was placed in a TCC and SAP used due to concerns about the excessive drainage. With the drainage controlled, maceration resolved and offloading successfully managed, he went on to heal completely. |
 |
| Case History 2 64 year old IDDM with a history of a Diabetic Neuropathic foot ulcer of the plantar heel. He had undergone surgery years before leaving him with a soft tissue deformity predisposing him to recurrent ulcers. |
Cource of Treatment An aggressive debridement was performed with no bone exposure noted. He had moderate serous drainage from the ulcer and so SF was used to control the drainage without creating a dry wound base. TCC was performed weekly with changes of the SF dressing. With the drainage controlled and offloading accomplished, he went on to heal completely. |
 |
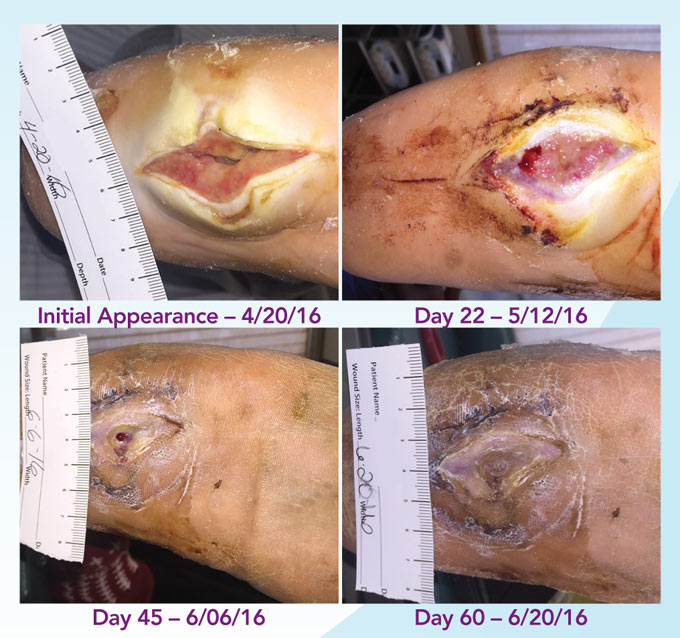
| Case History 3 A 64 year old female with advanced rheumatoid arthritis and foot deformity presented with a 6 month history of a nonhealing ulcer of the right plantar foot. A surgery to correct this had incisional dehiscence. Topical dressings and an offloading boot were previously used unsuccessfully. |
Course of Treatment An aggressive debridement was performed with no bone exposure noted. Her significant serous drainage was treated with SAP and TCC applied weekly for offloading. Over the next several weeks, the drainage decreased and the dressing was changed to SF due to decreasing wound drainage. With the drainage controlled and offloading in place, she went on to heal completely. |
 |
References
1. Hurlow J, Couch K, Laforet K, Bolton L, Metcalf D, Bowler P. (2015) “Clinical Biofilms: A Challenging Frontier in Wound Care”. Adv Wound Care (New Rochelle) 4(5): 295–301.
* KerraFoam is a registered trademark of Crawford Woundcare Ltd. † KerraMax Care is a registered trademark of Crawford Woundcare Ltd.
‡ Total Contact Casting Kits by M-Med, Mebane, NC., supplied at no charge for this case series.
This poster abstract is funded and supported by Crawford Healthcare Inc.
© Copyright Crawford Healthcare Ltd, 2016. This literature and product report is supported and funded by Crawford Healthcare Ltd. 2016
If you find WoundCareWeekly.com of value please consider a monthly donation to help cover expenses and keep this website going.